Typical day in Anaesthetics
Click on the heading below to find out what they might be doing at that specific point in the day.
As with any role within the NHS confidentiality, data protection and security is paramount before entering any clinical environment.  Usually entry will require authentication via security access passport, security codes or even buzzing to gain entry onto the premises. A professional attitude is vital and staff (including students) have a certain obligations to uphold when entering the clinical setting.
Usually entry will require authentication via security access passport, security codes or even buzzing to gain entry onto the premises. A professional attitude is vital and staff (including students) have a certain obligations to uphold when entering the clinical setting.
Shift patterns may vary where some may start work earlier than others dependant on duties for that day. usually Anaesthetics may start first with Recovery starting later and probably finishing later dependant on the patients needs.
As a student you will be required to work Monday to Friday and you may be expected to work 'out of hours' to experience emergency and trauma care.
 On entering the department staff will proceed to the changing rooms in preparation for entering a clean environment. 'Dress codes' and cleanliness are major protectors against hospital infections, and proper preparation to enter a surgical environment is vital. This will mean the removal of all jewellery, with few exemptions and the donning of theatre scrubs as per local hospital policy.
On entering the department staff will proceed to the changing rooms in preparation for entering a clean environment. 'Dress codes' and cleanliness are major protectors against hospital infections, and proper preparation to enter a surgical environment is vital. This will mean the removal of all jewellery, with few exemptions and the donning of theatre scrubs as per local hospital policy.
Dependant on speciality this may vary from Scrubs and shoes, to in some case full scrubs, shoes, hat and mask. Scrubs are supplied by the Trust whilst specialist theatre shoes are worn to minimise cross contamination from the outside world.
Many operating departments work on the policy the closer to the patient operating room the cleaner the environment.
One of the biggest impacting factors on daily workload is the constant changing of duties on a day to day basis. Many times you will leave the previous day thinking you are in one theatre and the next morning due to emergencies for example everything may have changed, not only might you be in another theatre, but it might even be an entirely different speciality. Generally you will be where planned but with increasing experience comes increasing responsibility to the service.
To meet these challenges communication punctuality, organisation and team working are essential qualities in a potential ODP.
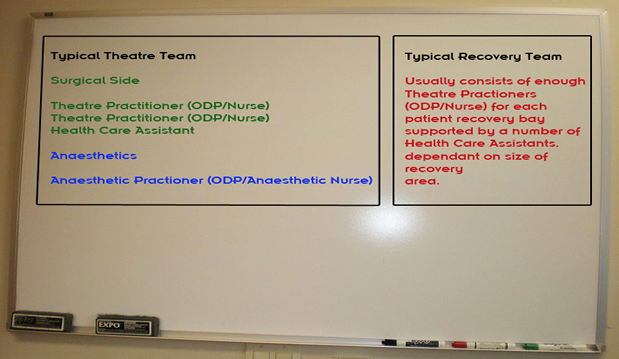
These are suggested total and do not represent any individual organisation, as many will have their own policies and procedures to maintain.
The anaesthetic practitioner, after collecting the operating list containing all the session procedures, order of play and specialist requirements will start to prepare the anaesthetic area. 
These checks might include;
- Checking anaesthetic equipment
- Preparing work surfaces
- Ensuring all specialist equipment is in situ
- Making sure all the drugs required for the list are available and are at hand
- Ensuring that emergency equipment is available if required
- Checking that the operating table is correct and set up appropriately for the first case.
Communication amongst the Multi Disciplinary Team (MDT) is paramount at this stage. It is vital that the team communicate with each other to confirm that all the necessary equipment is available when required, all the staff are ready to commence the operating list.
After everything has been prepared, all the staff have been accounted for and are present an MDT decision is made to send for the first patient. This is usually an anaesthetic duty, but can and will at some point involve the surgical team.
Greeting the patient and providing holistic care is paramount to good patient care. Communication is vital as the patient is handed over to theatre staff from the ward. Policies and procedures are paramount for patient safety. Checks include;
- Name
- Hospital ID
- Previous medical history
- Current medical issues
- Understanding of what is happening
- Consent form
Only when everything has been checked can a procedure start which usually means connecting the patient to monitoring, such as blood pressure, ECG, and pulse oximetry. Different procedures may require more invasive techniques such as an arterial line for constant pressure monitoring.
Following checking procedures the ODP will assist the Anaesthetist to prepare the patient for surgery. An anaesthetic covers three basic functions. They are awareness, analgesia and relaxation and dependant on the severity of the operating procedure differing levels of each will be required.
Patients generally require venous access and in some case arterial access as well, all of which require an ODP either to assist in their application or through extended scope actually performing the task. The Anaesthetist and the ODP work as a team ensuring that the patient is in the best condition required by the surgeon to gain access and perform the surgery or for a patients particular medical demands.
Once the patient has been prepared they are taken into the operating theatre for the surgical procedure to be carried out.
 Patient safety comes first. With this in mind the ODP assists the anaesthetist in connecting the patient to all the relevant monitors and anaesthetic equipment to ensure that they are comfortable and in a state of readiness for the surgical procedure.
Patient safety comes first. With this in mind the ODP assists the anaesthetist in connecting the patient to all the relevant monitors and anaesthetic equipment to ensure that they are comfortable and in a state of readiness for the surgical procedure.
The team will then employ well practiced procedures to transfer the patient to the operating table and then into position for the surgery. There are many different positions which range from the simple supine position to the complexity of other positions, prone being a good example (patient is face down).
Once positioned correctly other equipment required for the procedure is introduced dependant on the needs and requirements of the surgical procedure to be performed. Equipment may include Diathermy Laparoscopic equipment Suction.
At this point prior to surgery a final check is made to
ensure that we have the correct patient, who is having the correct planned procedure and if a side is designated (right
leg for example) that we are working on the correct site. The World Health Organisation checklist has been
adopted by many organisations as the gold standard for
prevention of surgical wrong site/procedure mistakes.
Once all the checks have been completed, which includes final mandatory checks and the procedure has commenced the ODP will assist the Anaesthetist to maintain the patients state, ensuring that vital signs and patient comfort is maintained.
They will also have to prepare the anaesthetic room for the next patient. This will include the cleaning of all work surfaces, including the removal of any blood spillages and checking of all the equipment and disposal of sundries, such as used swabs and clinical waste from the present procedure in preparation for the next patient on the operating list.
During the procedure the rest of the team which includes the anaesthetic ODP, the circulating person and dependant on the organisation and the size and workload of the department possibly the recovery person will support the surgical and anaesthetic teams, ensuring patient and staff safety throughout. Tasks may include, moving the light, connecting fluids, adjusting insufflators, checking swabs and much more, dependant on the need at the time. Counts of all instruments and consumables will take place throughout at the procedure at different points and can include all staff within that particular theatre. At times communication with other departments may be necessary, such as X-ray, labs, the ward, dependant on the procedural demands of a particular surgery.
Since the human body can develop many illnesses that requires a surgical intervention the surgical procedures can be quite varied in a number of different ways. Each surgical procedure will have its own demands both emotional and physical on the staff and patient. They can range from quick fast flowing operating lists where the physical demand is high coupled with high emotional impact such and a suction termination of pregnancy, to a long and drawn out surgical intervention that although does not have a high impact on all the team, physically could be very arduous and fatigue may be an issue. Standing at an operating table in one spot for two to three hours can have its own stresses. Tensions can run high in the stressful environment of an operating theatre where different personalities have to work closely together for the best outcome for the patient in their care, regardless of personal culture and beliefs.
Exposure to gases, unpleasant odours, blood splashes are all part of a daily routine. Risk from sharps injuries and the dangers that are present when dealing with members of the public, remember that in this environment, the patients we see are for the most part experiencing the worst day of their lives, and we do not just treat the people we are happy to treat. Everybody deserves a good health care, no matter what their cultural or society standing. Of course there are the pleasant days such as being part of a caesarean section and witnessing the start of a new life.
 Recovery from the surgical procedure and the anaesthetic begins on the operating table. Once all the counts have been completed satisfactorily, the patient cleaned and all the appropriate aftercare dressings applied the patient is slowly reversed from the anaesthetic. The main function of the team here is to prepare the patient for transfer to the recovery area.
Recovery from the surgical procedure and the anaesthetic begins on the operating table. Once all the counts have been completed satisfactorily, the patient cleaned and all the appropriate aftercare dressings applied the patient is slowly reversed from the anaesthetic. The main function of the team here is to prepare the patient for transfer to the recovery area.
The Anaesthetic ODP will assist the Anaesthetist in making sure the patient is both comfortable and pain free. In some organisation this role may be carried out by a recovery ODP. The surgical team will also assist in the safe hand over of patient specific information to the next treatment area.
Once the patient is able to be transfer and leaves the theatre, preparation for the next procedure begins.
This is everyone's role with in the team. All clinical waste from the previous procedure needs to be removed safely following organisational protocols for hazardous waste. All surfaces must be cleaned and prepared for the next case.
In the case of anaesthetics this will include preparation of the anaesthetic machine which may require a complete recheck to ensure all is in working order.
The operating table may need altering for different procedures, in the case of Orthopaedics this may mean a completely new table as some procedures will need the traction attachments assembling.
New specialist equipment might be required. In the case of a general list the first case may have been an open procedure whilst the next could be laparoscopic .
In recovery this will mean cleaning and restocking of the different bays that the patients utilise.
The day can be tedious, hard working and sometimes downright boring, certainly there are the exciting times when people are desperately trying hard to save a life but they are few and far between. Standing for long periods whilst scrubbed or watching monitors during long cases observing no change in patient's vital signs are normal everyday occurrences in the life of an ODP. The role has it's rewards but sometimes staff can feel that much of their work is unchanging and sometimes feel that little recognition is awarded for all their efforts.
During winter periods it is normal to go to work in the dark and come home in the dark and sometimes not see daylight for a week simply as most operating departments are unusually placed in the basement and have no external windows.
The role is life changing in many ways so due consideration is required, the rewards as stated earlier are plentiful, but the cost can be at times be extreme.
